Abstract
Introduction: Bystander Cardiopulmonary Resuscitation (CPR) has been recognized as a critical component in the survival of out-of-hospital cardiac arrest (OHCA); likewise, time is a factor in the effectiveness of CPR. Pre-arrival instructions (PAIs) for CPR performance by Emergency Medical Dispatchers (EMDs) increase the rate of bystander CPR and OHCA survival. While uncontrollable barriers to PAIs delivery exists, time to first compression (TTFC) remains a modifiable component of the EMD-caller interaction.
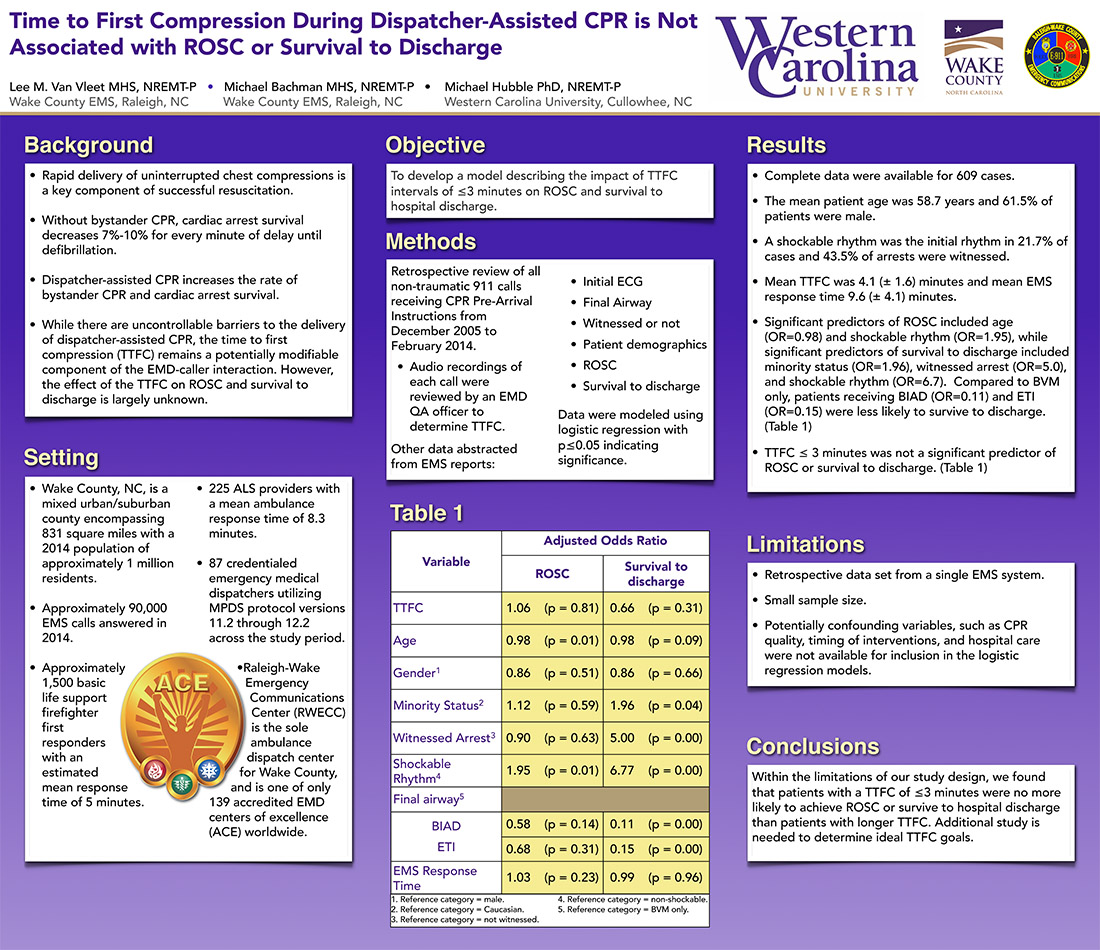
Objective: To develop a model describing the impact of TTFC intervals of ≤3 minutes on Return Of Spontaneous Circulation (ROSC) and survival to hospital discharge.
Methods: This retrospective review included all patients suffering non-traumatic cardiac arrest and receiving CPR PAIs in an urban/suburban Emergency Medical Services (EMS) system between December, 2005 and January, 2014. Audio recordings of all CPR PAI events were analyzed for TTFC. Additional data were abstracted from the EMS record including response time, initial EKG, final airway (Bag Valve Mask (BVM) only, Blind Insertion Airway Device (BIAD), or endotracheal intubation (ETI)), witnessed arrest, patient demographics, ROSC, and survival to discharge. Data were modeled using logistic regression with p≤0.05 indicating significance.
Results: Complete data for 609 cardiac arrests; mean age of 58.7 years were analyzed. Mean EMS response time was 9.6 minutes, 43.5% were witnessed arrests, 21.7% had shockable initial rhythms, and 61.5% were males. ROSC was achieved in 61.3% and 10.0% survived to hospital discharge. With respect to ROSC, significant predictors included age (Odds Ratio (OR) =0.98, p=0.01) and shockable rhythm (OR=1.95, p=0.01). All other predictors were non-significant, including TTFC interval ≤3 minutes (OR=1.06, p=0.81). Independent predictors of survival to discharge included minority status (OR=1.96, p=0.04), witnessed arrest (OR=5.0, p<0.01), and shockable rhythm (OR=6.7, p<0.01). Compared to BVM only, patients receiving BIAD (OR=0.11, p<0.01) and ETI (OR=0.15, p<0.01) were less likely to survive. TTFC interval ≤3 minutes was not associated with survival to discharge (OR=0.662, p=0.32).
Conclusion: Within the limitations of our study design, we found that patients with a TTFC of ≤3 minutes were no more likely to achieve ROSC or survive to hospital discharge than patients with longer TTFC. Additional study should determine ideal TTFC goals.
